- Home
- About Cancer
- Managing side effects
- Sexuality, intimacy and cancer
- Sex and your body
Sex and your body
Discover the connection between sex and your body, including libido, emotional wellness, and the sexual response cycle.
Learn more about:
- Overview
- The sexual response
- Erogenous zones
- About sex hormones
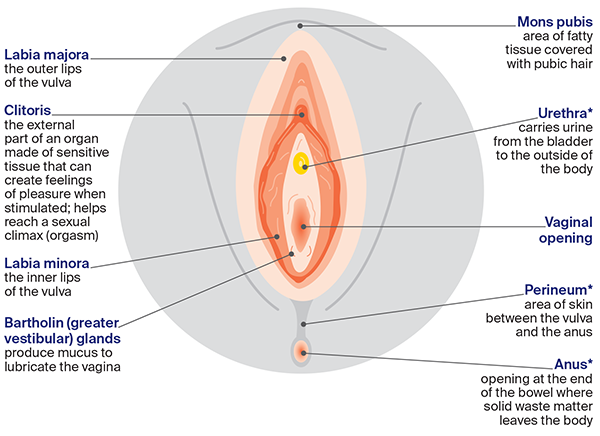
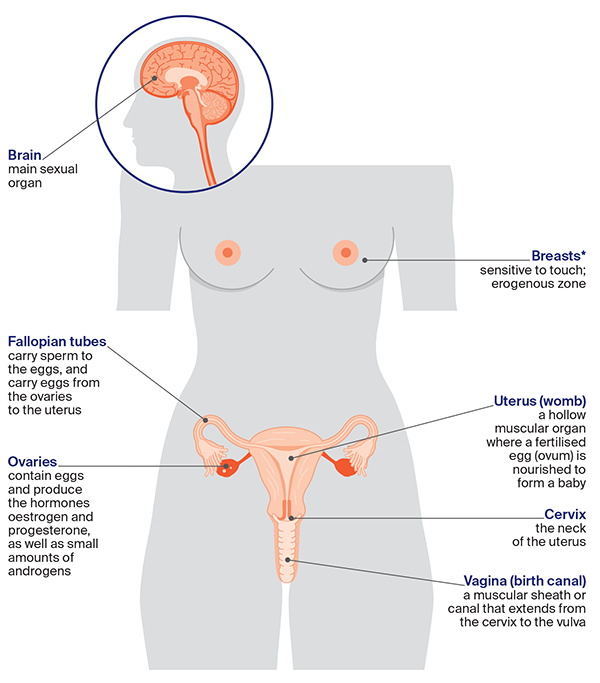
- The female sexual and reproductive anatomy
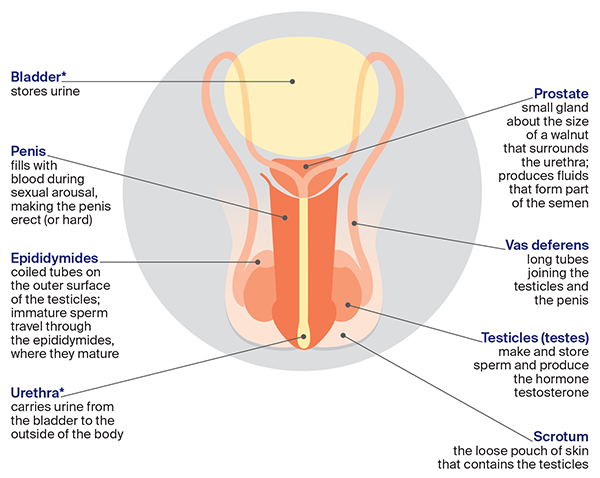
- The male sexual and reproductive anatomy
Overview
Feeling like you want to have sex is called your sexual desire or libido. It is affected by your physical and emotional wellbeing, levels of sex hormones, relationship and body image, as well as the need to express love, give and receive pleasure, and connect with others. Some cancer treatments can reduce your desire or libido.
The sexual response
Knowing what happens to your body during sex can help you to understand any changes. This is called the sexual response cycle. It includes several different phases: desire (wanting sex), arousal (feeling excited or turned on), plateau, orgasm and resolution. These phases are the same for all genders, but the timing can be different for each person. You may not go through every stage (e.g. you may not orgasm).
Arousal can begin in 2 ways – from the brain (psychogenic), or by touch (reflexogenic). The brain controls your interest in sex through memories, feelings and thoughts – what you see, smell, touch, taste, hear and imagine. If you are touched on the genitals or a sensitive area, this can start the process of feeling like sex.
Erogenous zones
Areas of the body that make you feel aroused when touched are called erogenous zones. The main ones are the clitoris, labia, vagina, penis, scrotum and anus. Other erogenous zones include the breasts, nipples, chest, mouth, ears, neck and inner thighs.
Cancer or its treatment may change how these areas feel. They may become more sensitive or they may lose some sensation.
About sex hormones
Hormones are made naturally in your body. They control many functions, including how you grow and develop, and your ability to have children (your fertility). Generally, males have more testosterone and females have more oestrogen and progesterone. These hormones may vary for transgender or intersex people.
Low sex hormones or sudden hormone changes can affect your mood or lead to depression.
Androgens (male sex hormones)
The main androgen is testosterone, which is made mostly in the testicles. It’s also produced in small amounts by everyone’s adrenal glands (including females).
Some cancer treatments (e.g. for prostate cancer) use testosterone- depriving drugs called androgen deprivation therapy or ADT. These medicines can cause erection problems, fatigue and low interest in sex (libido). They may also increase body fat and change your body image. If you are on ADT, exercise may help you to maintain muscle mass and bone strength, and support your mental health.
The ovaries also make small amounts of androgens, which may help female sexual wellbeing. Androgens often drop during and after chemotherapy, and can decrease suddenly if the ovaries are removed.
Oestrogen and progesterone (female sex hormones)
Oestrogen keeps the vagina moist and stretchy. It helps with concentration and overall wellbeing. Progesterone controls reproduction (periods and pregnancy). These hormones are mostly made in the ovaries before menopause, but some continue to be made in the adrenal glands. Some cancer treatments may lower these hormones or cause early menopause.
The female sexual and reproductive anatomy
The female sexual and reproductive organs are found inside (internal) and outside (external) the body. You may or may not have some of these organs.
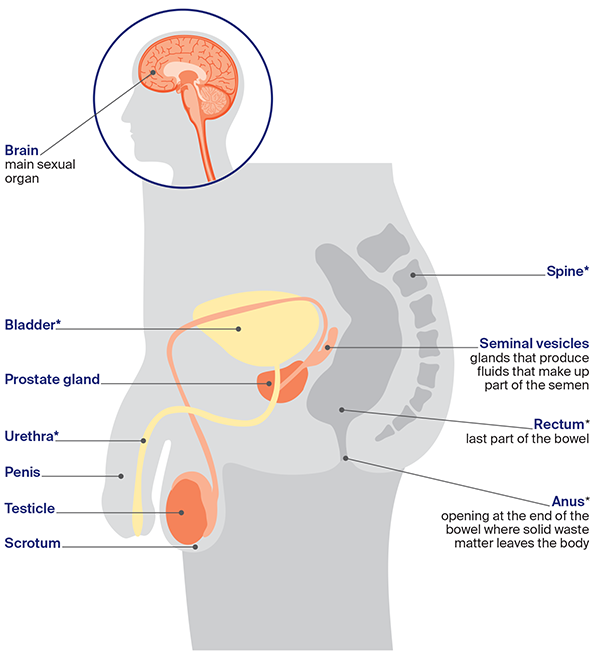
The male sexual and reproductive anatomy
The male sexual and reproductive organs are found both inside (internal) and outside (external) the body. You may or may not have some of these organs.
→ READ MORE: Treatment side effects
Podcast: Sex and Cancer
Listen to more of our podcast for people affected by cancer
More resources
Dr Michael Lowy, Sexual Health Physician, Sydney Men’s Health, NSW; Gregory Bock, Clinical Nurse Consultant – Oncology Coordinator, Urology Cancer Nurse Coordination Service, Cancer Network WA; Anita Brown-Major, Occupational Therapist and Director, Thrive Rehab, VIC; Helena Green, Psychosexual Therapist and Clinical Sexologist, Insync for Life Psychology and Women Centre, WA; Dr Lisa Mackenzie, Clinical Psychologist, HNE Centre for Gynaecological Cancer, Hunter New England Local Health District, NSW; Dr Tonia Mezzini, Sexual Health Physician, East Obstetrics and Gynaecology, SA; Sophie Otto, Prostate Cancer Nurse Consultant – Central Adelaide Local Health Network (CALHN), SA; Giovanna Raco, 13 11 20 Consultant, Cancer Council Victoria; Kath Schubach, Urology Nurse Practitioner, VIC; Emily Stevens, Gynaecology Oncology Clinical Nurse Consultant, Southern Adelaide Local Health Network, Flinders Medical Centre, SA; Anja Vukovic, Clinical Specialist Social Worker, Gynaecological Oncology, Westmead Hospital, NSW; Alan White, Consumer; Kathleen Wilkins, Consumer; Merran Williams, Consumer.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.