- Home
- Cancer Information
- Managing side effects
- Sexuality, intimacy and cancer
- The sexual response
The sexual response
Your interest in having sex is also called your sexual desire or libido. It is affected by your physical and emotional wellbeing, relationship satisfaction, body image, and levels of sex hormones, as well as the need to express love, give and receive pleasure, and create connection.
Learn more about:
- Overview
- Stages of the sexual response cycle
- Erogenous zones
- The role of hormones
- The female sexual and reproductive anatomy
- The male sexual anatomy
Overview
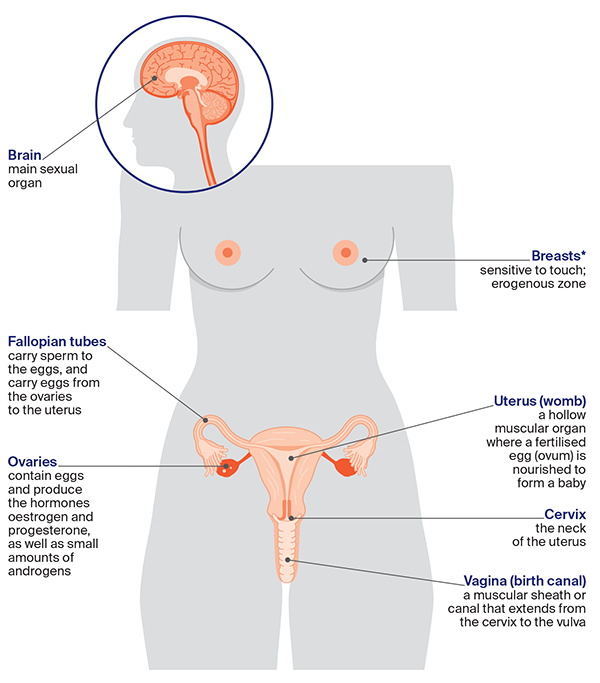
Sexuality starts in the brain. It is responsible for making you feel interested in sex through your memories, feelings and imagination. These thoughts are created by what you see, smell, touch, taste, hear and remember. The mind is also responsible for your body image – how you feel about your body and how you think it looks.
Stages of the sexual response cycle
Understanding what is happening to your body during sexual activity can be helpful. The sexual response cycle can be described in different ways. A common model includes several phases: desire, arousal (excitement), plateau, orgasm and resolution. These phases are the same for all sexes. The timing can be different for each person, and you may not go through all the stages. For example, you may experience pleasure without having an orgasm.
Erogenous zones
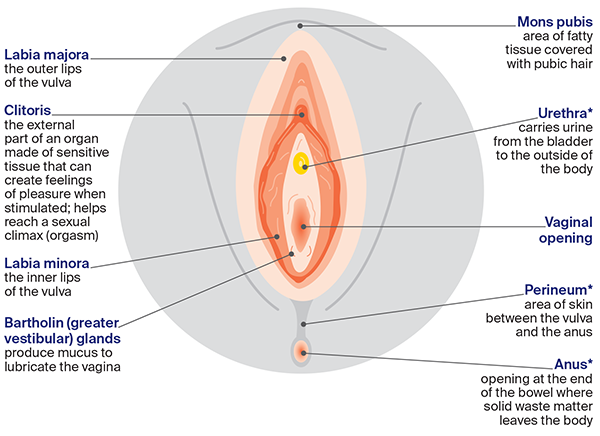
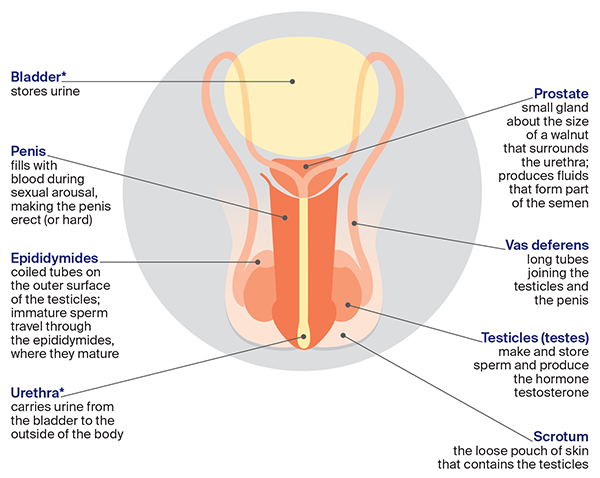
Areas of the body that can make you feel excited or aroused when they’re touched or stimulated are known as erogenous zones.
The main erogenous zones for most people are in the genital area: the clitoris, labia, vagina, penis, scrotum and anus. Other erogenous zones include the breasts, nipples, chest, mouth, ears, neck and inner thighs.
The role of hormones
Hormones are substances that affect how your body works. They act as messengers carrying information and instructions from one group of cells to another. Hormones control many of the body’s functions, including how you grow, develop and reproduce. Everyone has hormones in their bodies in various levels: generally, men have more testosterone and women have more oestrogen and progesterone. This may vary for transgender or intersex people.
Androgens
These are often called male sex hormones. The major androgen is testosterone, which is produced mostly in the testicles, but also in the male and female adrenal glands. It causes the reproductive organs and other sexual characteristics, such as body/facial hair and a deep voice, to develop. Some cancer treatments (e.g. for prostate cancer) include testosterone-blocking drugs (androgen deprivation therapy or ADT). These drugs can affect the ability to get or keep an erection and reduce your desire for sex. They may also increase body fat, changing your body image, and this can affect how you feel about sex.
The ovaries make small amounts of androgens, which may support female sexual wellbeing. The levels of androgens decrease during and after chemotherapy, and can drop suddenly if the ovaries are removed.
Oestrogen and progesterone
These are often called the female sex hormones. Oestrogen keeps the vagina moist and supple and contributes to feelings of wellbeing and concentration, while progesterone controls reproduction. Both hormones are produced mostly in the ovaries until menopause, when the ovaries stop releasing eggs and periods end. Small amounts of oestrogen and progesterone are made in the adrenal glands before and after menopause. Some cancer treatments can affect these hormone levels, causing early menopause or menopause-like symptoms.
The female sexual and reproductive anatomy
The female sexual and reproductive organs are found inside (internal) and outside (external) the body. You may or may not have some of these organs.
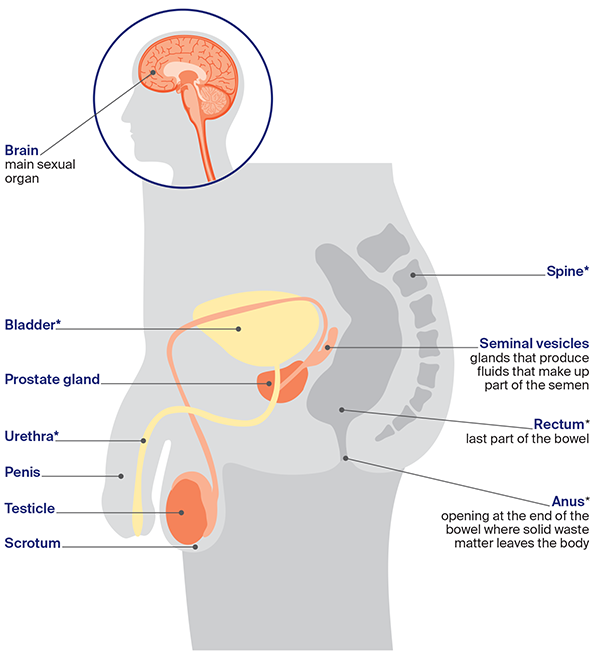
The male sexual and reproductive anatomy
The male sexual and reproductive organs are found both inside (internal) and outside (external) the body. You may or may not have some of these organs.
→ READ MORE: Treatment side effects
Podcast: Sex and Cancer
Listen to more of our podcast for people affected by cancer
More resources
Dr Margaret McGrath, Head of Discipline: Occupational Therapy, Sydney School of Health Sciences, The University of Sydney, NSW; Yvette Adams, Consumer; Dr Kimberley Allison, Out with Cancer study, Western Sydney University, NSW; Andreea Ardeleanu, Mental Health Accredited Social Worker, Cancer Counselling Service, Canberra Health Service, ACT; Kate Barber, 13 11 20 Consultant, Cancer Council Victoria; Dr Kerrie Clover, Senior Clinical Psychologist, Psycho-Oncology Service, Calvary Mater Newcastle, NSW; Maree Grier, Senior Clinical Psychologist, Royal Brisbane and Women’s Hospital, QLD; Mark Jenkin, Consumer; Bronwyn Jennings, Gynaecology Oncology Clinical Nurse Consultant, Mater Health, QLD; Dr Rosalie Power, Out with Cancer study, Western Sydney University, NSW; Dr Margaret Redelman OAM, Medical Practitioner and Clinical Psychosexual Therapist, Sydney, NSW; Kerry Santoro, Prostate Cancer Specialist Nurse Consultant, Southern Adelaide Local Health Network, SA; Simone Sheridan, Sexual Health Nurse Consultant, Sexual Health Services – Austin Health, Royal Talbot Rehabilitation Centre, VIC; Prof Jane Ussher, Chair, Women’s Heath Psychology and Chief Investigator, Out with Cancer study, Western Sydney University, NSW; Paula Watt, Clinical Psychologist, WOMEN Centre, WA.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.
Need to talk?
Support services
Coping with cancer?
Speak to a health professional or to someone who has been there, or find a support group or forum
Life after cancer treatment
Webinars, exercise and nutrition, sexuality programs, and back-to-work support
Cancer information
Your coping toolbox
Strategies for managing difficult situations during and after cancer treatment
View our publications
Guides and fact sheets for people with cancer, their families and friends