- Home
- Cancer of the uterus
- Treatment
- Surgery
Surgery for cancer of the uterus
Cancer of the uterus (endometrial cancer) is usually treated with an operation that removes the uterus and cervix (total hysterectomy), along with both fallopian tubes and ovaries (bilateral salpingo-oophorectomy). If your ovaries appear normal, you don’t have any risk factors, and it is an early-stage, low-grade cancer, you may be able to keep your ovaries. If the cancer has spread beyond the cervix, the surgeon may also remove a small part of the upper vagina and the ligaments supporting the cervix.
Learn more about:
- Total hysterectomy and bilateral salpingo-oophorectomy
- How the surgery is done
- Treatment of lymph nodes
- What to expect after surgery
- Taking care of yourself at home after a hysterectomy
- Side effects of surgery
Total hysterectomy and bilateral salpingo-oophorectomy
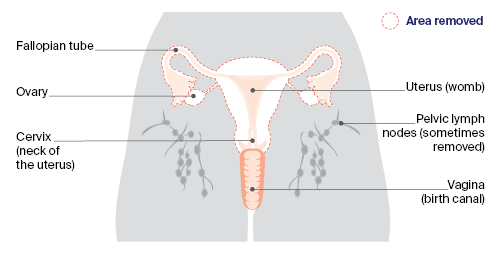
Most people with cancer of the uterus will have this operation, which removes the uterus, cervix, fallopian tubes and ovaries (as shown by the dotted line). Sometimes one or more pelvic lymph nodes are also removed to help with staging.
A pathologist examines all removed tissue and fluids. The results will help confirm the type of cancer of the uterus, if it has spread (metastasised), and its stage and grade. The cancer may also be tested for particular gene changes.
How the surgery is done
The surgery will be performed under a general anaesthetic. Your surgeon will discuss the most appropriate surgery for you, and explain the risks and benefits.
The type of hysterectomy you have depends on a number of factors, such as:
- your age and build
- the size of your uterus
- the tumour size
- the surgeon’s specialty and experience.
See below for more information about the different types of surgery you might have.
Types of surgery
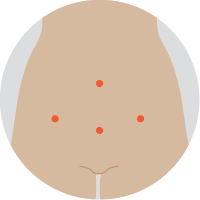 | Keyhole surgeryAlso called a laparoscopic hysterectomy, a surgeon inserts a laparoscope (thin tube with light and camera) and instruments through about 4 small cuts in the abdomen. The uterus and other organs are removed through the vagina. |
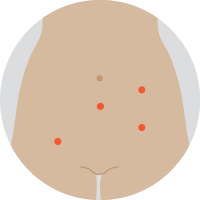 | Robotic-assisted hysterectomyThis is a special form of keyhole surgery. The instruments and camera are inserted through about 4 small cuts, and controlled by robotic arms guided by the surgeon, who sits next to the operating table. |
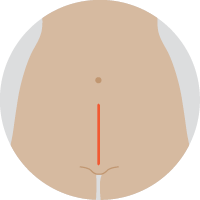 | Open surgeryThis surgery (also called abdominal hysterectomy or laparotomy) is done through the abdomen. A cut is usually made from the pubic area to the bellybutton. The uterus and other organs are then removed. |
Treatment of lymph nodes
Cancer cells can spread from the uterus to the pelvic lymph nodes. If this occurs, your doctor may recommend you have additional treatment after surgery, such as chemotherapy or radiation therapy.
Lymph nodes may be checked in 2 ways:
- Lymphadenectomy (lymph node dissection) – For more advanced or higher-grade tumours, the surgeon may remove some lymph nodes from the pelvic area to see if the cancer has spread beyond the uterus.
- Sentinel lymph node biopsy – This test helps to identify the pelvic lymph node that the cancer is most likely to spread to first (the sentinel node). While you are under anaesthetic, your doctor will inject a dye into the cervix. The dye will flow to the sentinel lymph node, which will be removed for testing. Sentinel lymph node biopsies are available only in some treatment centres.
Podcast: Making Treatment Decisions
Listen to more of our podcast for people affected by cancer
→ READ MORE: What to expect after surgery
More resources
A/Prof Orla McNally, Consultant Gynaecological Oncologist, Director Oncology/Dysplasia, Royal Women’s Hospital, Honorary Clinical Associate Professor, University of Melbourne, and Director of Gynaecology Tumour Stream, Victorian Comprehensive Cancer Centre, VIC; A/Prof Yoland Antill, Medical Oncologist, Peninsula Health, Parkville Familial Cancer Centre, Cabrini Health and Monash University, VIC; Grace Guerzoni, Consumer; Zeina Hayes, 13 11 20 Consultant, Cancer Council Victoria; Bronwyn Jennings, Gynaecology Oncology Clinical Nurse Consultant, Mater Hospital Brisbane, QLD; A/Prof Christopher Milross, Director of Mission and Radiation Oncologist, Chris O’Brien Lifehouse, NSW; Mariad O’Gorman, Clinical Psychologist, Liverpool Cancer Therapy Centre and Bankstown Cancer Centre, NSW.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.
Need to talk?
Support services
Coping with cancer?
Speak to a health professional or someone who has been there, or find a support group or forum
Work and cancer
Information for employees, employers and workplaces dealing with cancer
Cancer information
Recovering from surgery
What to expect in the hospital recovery room and ward
Supporting someone having surgery
Tips for the support person and visitors

