- Home
- Vulvar cancer
- About vulvar cancer
About vulvar cancer
Vulvar cancer is the abnormal growth of cells in any part of the vulva. It is also called vulval cancer or cancer of the vulva.
Vulvar cancer most commonly develops in the skin of the labia majora, labia minora and the perineum. Less often, it involves the clitoris, mons pubis or Bartholin glands. As the cancer grows, it can spread to areas near the vulva, such as the vagina, bladder or anus.
Learn more about:
- Types of vulvar cancer
- The vulva
- Who gets vulvar cancer?
- What causes vulvar cancer?
- What are precancerous vulvar cell changes?
What are the types of vulvar cancer?
The types of vulvar cancer are named after the cells they start in.
| squamous cell carcinoma (SCC) |
|
| vulvar (mucosal) melanoma |
|
There are also rarer types of vulvar cancer. These include sarcomas, adenocarcinomas, Paget disease of the vulva, and basal cell carcinomas (BCCs).
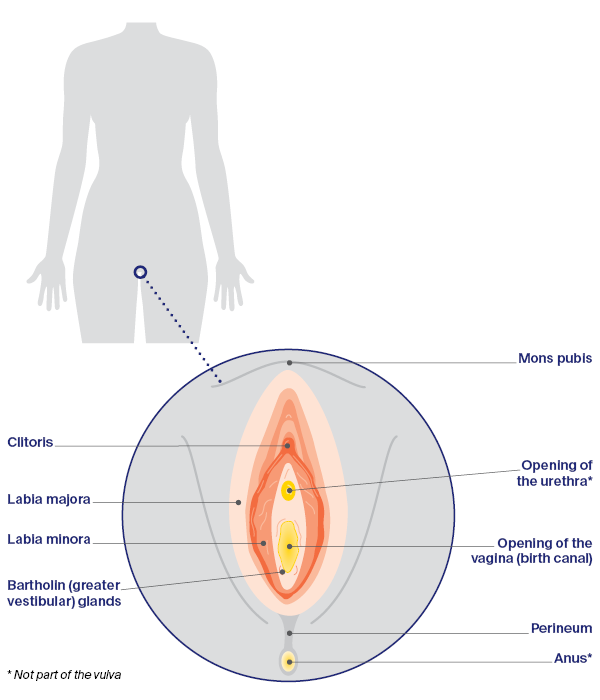
The vulva
The vulva is a general term for a female’s external sexual organs (genitals). The main parts of the vulva are the:
- mons pubis – area of fatty tissue covered with pubic hair
- labia majora – outer lips of the vulva
- labia minora – inner lips of the vulva
- clitoris – external part of an organ made of sensitive tissue that can create feelings of pleasure when stimulated; helps reach a sexual climax (orgasm)
- Bartholin (greater vestibular) glands – produce mucus to lubricate the vagina.
Below the clitoris is the urethra, for passing urine. Further down is the entrance to the vagina, and behind that is the anus. The area of skin between the vagina and the anus is called the perineum.
Parts of the vulva
Who gets vulvar cancer?
Vulvar cancer is rare – about 420 women are diagnosed each year in Australia. It is more likely to affect women who have gone through menopause (stopped having periods), but it can occur at any age.
Anyone with a vulva can get vulvar cancer – women, transgender men, non-binary people and intersex people. For more information, speak to your doctor or see LGBTQI+ people and cancer.
What causes vulvar cancer?
The exact cause of vulvar cancer is unknown, but there are several things that increase the risk of developing it.
Vulvar squamous intraepithelial lesions (SIL)
Having vulvar SIL increases the risk of developing vulvar cancer. This condition changes the vulvar skin, and may cause itching, burning or soreness.
Human papillomavirus (HPV)
Many cases of vulvar cancer are caused by infection with HPV, which is a very common virus in people who are sexually active. HPV often causes no symptoms. Only some types of HPV cause cancer, and most people with HPV don’t develop vulvar or any other type of cancer. It can be many years between infection with HPV and the first signs of high grade squamous intraepithelial lesions (HSIL) or vulvar cancer.
Other risk factors
These include:
- the skin conditions vulvar lichen planus, vulvar lichen sclerosus or extramammary Paget disease
- having had an abnormal cervical screening test or cancer of the cervix or vagina
- smoking tobacco (which can make cancer more likely to develop in people with HPV)
- being aged over 70 (a little over half of all vulvar cancers are in women over 70)
- having a weakened immune system.
What are precancerous vulvar cell changes?
Sometimes the squamous cells in the vulva start to change. These changes may be precancerous. This means there is an area of abnormal tissue (a lesion) in the vulva that is not cancer, but may develop into cancer over time if left untreated.
These lesions are called vulvar squamous intraepithelial lesions (SIL). They can be classified as:
- low grade (LSIL), which may go away without treatment and is linked to human papillomavirus (HPV)
- high grade (HSIL), which may develop into vulvar cancer and is linked to HPV
- differentiated vulvar intraepithelial neoplasia (dVIN), which may develop into vulvar cancer and is not usually linked with HPV but is linked with the skin condition lichen sclerosus.
Most cases of vulvar SIL don’t develop into vulvar cancer. Your doctor will explain the treatment options suitable for you.
→ READ MORE: Vulvar cancer symptoms
More resources
Prof Alison Brand AM, Director, Gynaecological Oncology, Westmead Hospital, NSW; Kim Hobbs, Clinical Specialist Social Worker, Gynaecological Cancer, Westmead Hospital, NSW; Dr Ming-Yin Lin, Radiation Oncologist, Peter MacCallum Cancer Centre, VIC; Dr Lisa Mackenzie, Clinical Psychologist Registrar, HNE Centre for Gynaecological Cancer, Hunter New England Local Health District, NSW; Anne Mellon, CNC – Gynaecological Oncology, HNE Centre for Gynaecological Cancer, Hunter New England Local Health District, NSW; A/Prof Tarek Meniawy, Medical Oncologist, Sir Charles Gairdner Hospital and The University of Western Australia, WA; Dr Archana Rao, Gynaecological Oncologist, Senior Staff Specialist, Royal Brisbane and Women’s Hospital, QLD; Tara Redemski, Senior Physiotherapist – Cancer and Blood Disorders, Gold Coast University Hospital, QLD; Anita Tyrrell, Consumer; Maria Veale, 13 11 20 Consultant, Cancer Council QLD.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.
Need to talk?
Support services
Coping with cancer?
Speak to a health professional or to someone who has been there, or find a support group or forum
Need legal and financial assistance?
Pro bono services, financial and legal assistance, and no interest loans
Cancer information
What is cancer?
How cancer starts and spreads
Dealing with the diagnosis
Common reactions to a cancer diagnosis and how to find hope