- Home
- Chronic myeloid leukaemia (CML)
- Treatment
- Targeted therapy
Targeted therapy for CML
The main treatment for chronic myeloid leukaemia (CML) is a group of targeted therapy drugs called tyrosine kinase inhibitors (TKIs).
Learn more about:
- What are tyrosine kinase inhibitors (TKIs)?
- Continuing to take targeted therapy drugs
- Side effects of TKIs
- Video: What is targeted therapy?
- Podcast: Explaining immunotherapy & targeted therapy
What are tyrosine kinase inhibitors (TKIs)?
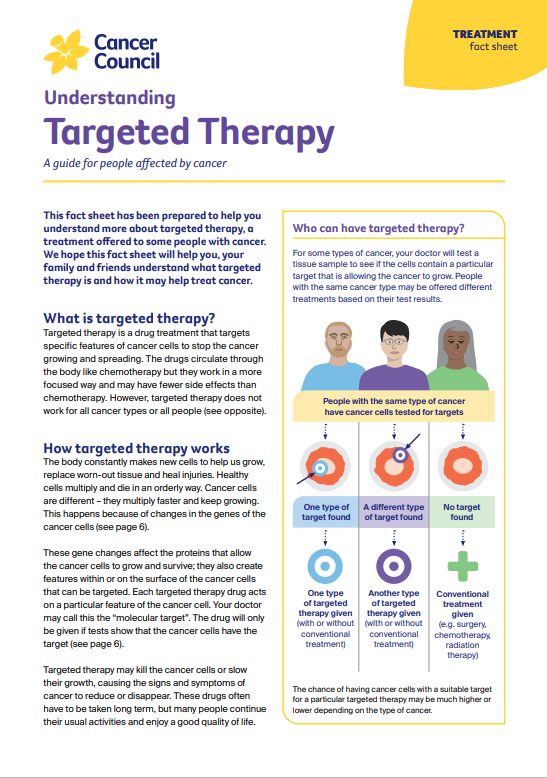
These drugs work by blocking a protein called tyrosine kinase. Tyrosine kinase tells the leukaemia cells to divide and grow. Without this signal, the cells die.
Each TKI works in a slightly different way. This means that if one TKI doesn’t control the CML or stops working for you, your doctor may increase the dose or switch you to another type of TKI.
You usually have TKIs as the first treatment, whether CML is in the chronic, accelerated or blast phase. The type of TKI you are prescribed will depend on several factors, including what other medical problems you have. In Australia, TKIs used for CML include imatinib, dasatinib, nilotinib and ponatinib. They are taken as tablets once or twice a day.
A new generation TKI, asciminib, is available for people with CML who cannot tolerate or have developed resistance to older TKIs.
Continuing to take targeted therapy drugs
TKIs can cause the signs and symptoms of CML to reduce or disappear. Most people are able to return to their usual activities. The drugs will need to be taken throughout your life, and you will need to have regular blood tests to check CML hasn’t returned.
Some people who have had an excellent response to a TKI for at least three years may be able to stop taking these drugs. If you are able to stop, you’ll need frequent check- ups. Half the people who stop have no further issues, and the other half have a relapse and need to start taking TKIs again.
Side effects of TKIs
The side effects of TKIs vary depending on the drug and how your body responds. Most side effects are mild and can be treated.
Common side effects may include:
- fatigue
- nausea and vomiting
- headache
- diarrhoea
- itchy skin rashes
- facial, hand or leg swelling
- anaemia, bruising or infections
- build-up of fluid around the lungs or heart.
In rare cases, TKIs can affect how the heart works, which can be life-threatening.
Tell your treatment team if you have any of these side effects and let them know if you have a history of heart disease. The team will monitor how you respond to the TKI and explain what side effects to watch out for or report, and who to contact after hours. For information about specific TKIs and their side effects, visit eviq.org.au.
Your doctor may be able to prescribe medicine to prevent or reduce side effects. Sometimes your doctor may have to change the dose of the TKI or give you a different TKI.
For more on this, see our general section on Targeted therapy.
Many TKIs, such as imatinib, are not safe to use during pregnancy or while breastfeeding. Ask your doctor for advice about contraception. If you become pregnant, let your medical team know immediately.
When I was first diagnosed I was put on imatinib, but I had severe side effects so my haematologist put me on dasatinib. I’ve been on this for over eight years with excellent results. As the leukaemia is still detected in the regular blood tests, there’s no plan to discontinue treatment in the foreseeable future.
Patricia
→ READ MORE: Chemotherapy for CML
Video: What is targeted therapy?
Watch this short video to learn more about targeted and immunotherapy
Podcast: Immunotherapy & Targeted Therapy
Listen to more episodes from our podcast for people affected by cancer
More resources
Dr Chun Kei Kris Ma, Clinical Haematologist, Western Sydney Local Health District (clinical update); Delphine Eggen, Consumer; Dr Robin Gasiorowski, Staff Specialist, Haematology, Concord Hospital; Karl A Jobburn, Haematology Clinical Nurse Consultant, Liverpool Hospital; Yvonne King, 13 11 20 Consultant, Cancer Council NSW; Heather Mackay, Clinical Nurse Consultant, Westmead Hospital; Jennifer Paton, Consumer.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.