Easy Read – Chemotherapy
Chemotherapy uses strong medicines to kill cancer. It is also called ‘chemo’. This information will help you understand what happens during chemotherapy and what side effects you may have.
On this page:
What is chemotherapy?
This information is about chemotherapy.
Chemotherapy is treatment for cancer.
The word ‘chemo’ also means chemotherapy.

Having chemotherapy can feel scary. You can ask your doctor questions about anything you do not understand.

Chemotherapy uses strong medicines to kill cancer.
How you get chemotherapy
There are many kinds of chemotherapy medicines.
Each person has different medicines. This is because some medicines work better for some types of cancer.
You may have one medicine or several medicines.
How you have chemotherapy
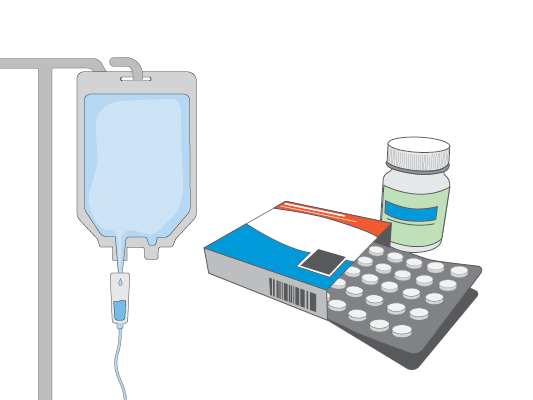
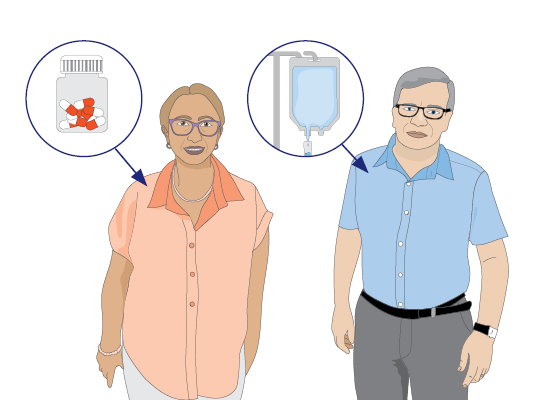
There are different ways to have chemotherapy.
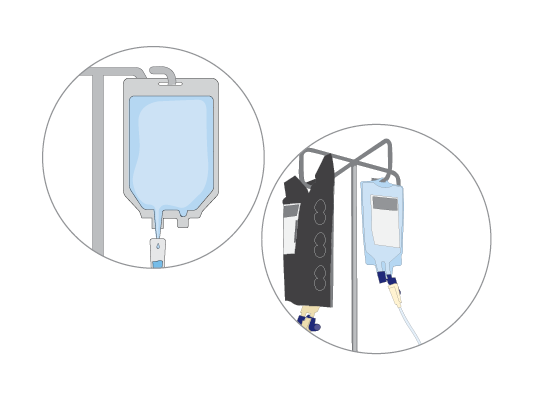
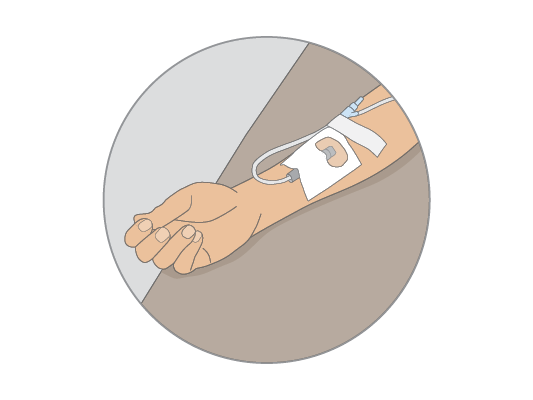
One way is through a vein in your arm. We call this intravenous (IV)
chemotherapy.
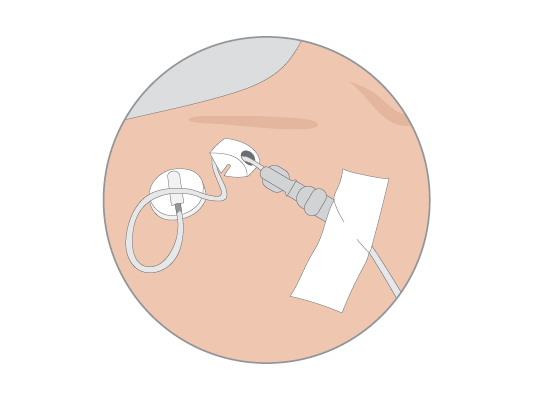
Sometimes you have chemotherapy through a vein in your chest.
You may also have chemotherapy as tablets that you swallow.

Where you have chemotherapy
You usually go to the hospital or treatment centre for chemotherapy.

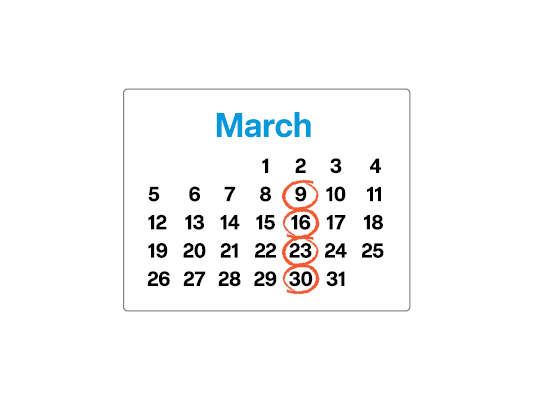
You may have treatment for a few weeks or a few months. This will depend on the chemotherapy medicines you are having.
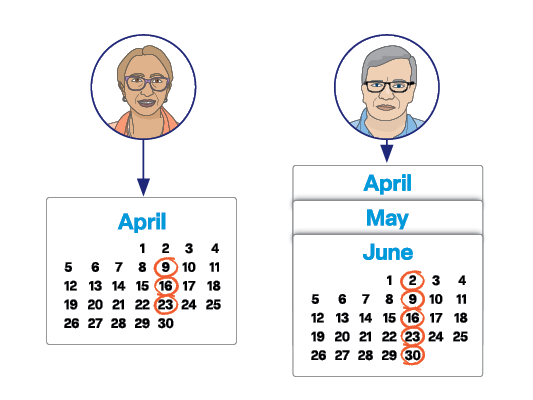
Your medical oncologist will tell you how many times you will have chemotherapy.
What happens during chemotherapy?
Different health professionals will look after you.

A doctor called a medical oncologist plans the chemotherapy.

A chemotherapy nurse will give you the chemotherapy medicines.

You will have a blood test before you start chemotherapy. They take blood using a small needle.
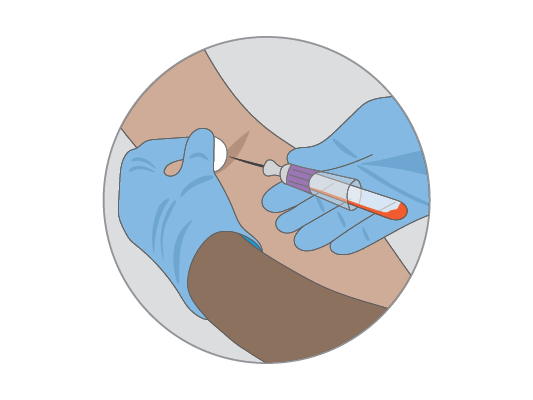
Having a blood test and having chemotherapy will not hurt.
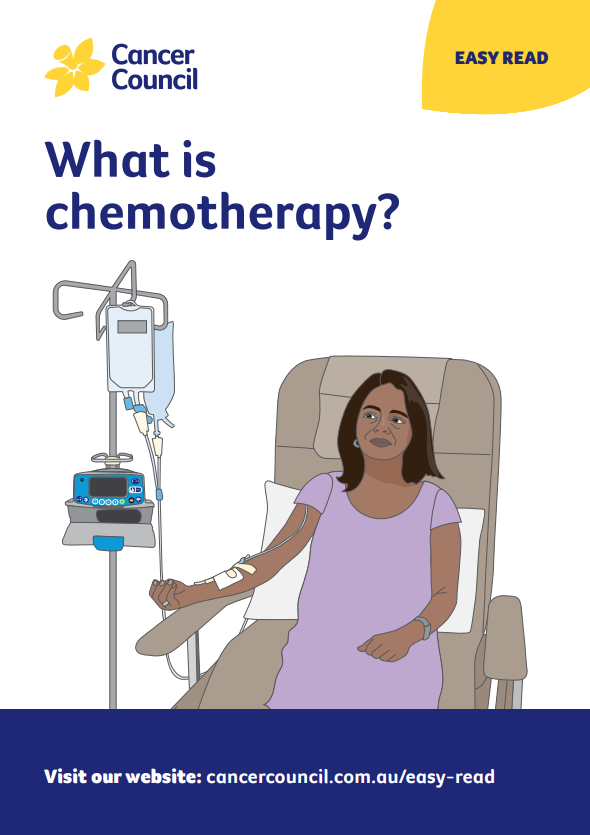
You sit in a comfortable chair and wear your own clothes.
It can take a few minutes or a few hours to have chemotherapy. It is
different for everyone.

Having chemotherapy can be boring. You can listen to music, read or play a game on your phone.
You can bring someone with you.

You can go home on the same day.
Your doctor will keep checking to see how the treatment is working. Sometimes they might change your treatment.

What are the side effects?
Some people feel sick when they have chemotherapy. We call these side effects.

Most people do not get all the side effects.
Side effects usually start a few days after you have chemotherapy.

The doctor will talk to you about side effects. They can suggest ways you can feel better.

Chemotherapy may make you feel very tired.

Some chemotherapy drugs make it hard to poo. We call this constipation.
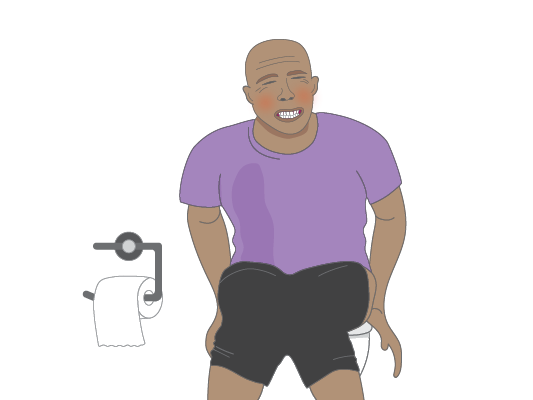
You may have runny poo. We call this diarrhoea.

Chemotherapy might make you feel like vomiting. We call this nausea.

You might get sores in your mouth.

Food may taste different. You may not enjoy eating as much.

Some chemotherapy medicines do not change your hair very much.

Some chemotherapy medicines make your hair fall out.

If your hair falls out, you can:
- wear a wig
- wear a headscarf
- leave your head uncovered.

Your hair will grow back when you stop chemotherapy.
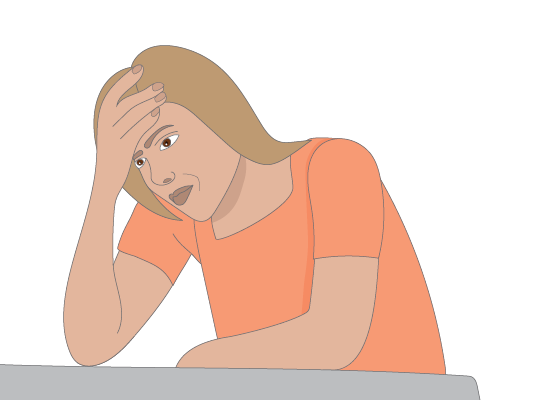
You may find it hard to focus and remember things.
We call this chemo brain or brain fog.
Chemotherapy may make it more likely to get a cold or flu.
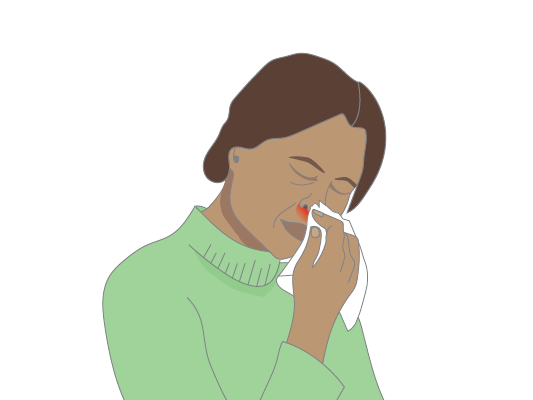
If your temperature goes over 38°C, you have a fever.
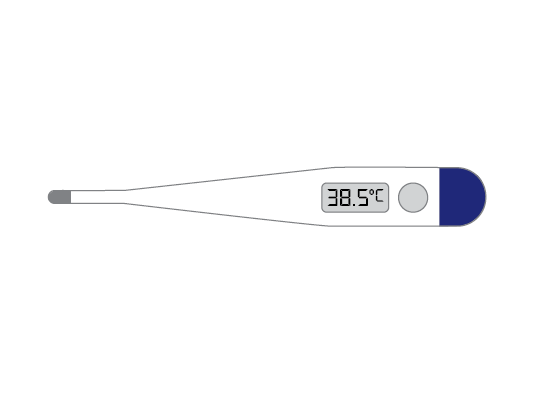
If you have a fever, call your oncologist.
If you feel very unwell, call 000 for an ambulance.
The ambulance will take you to hospital.

Coping with side effects
It might take a few weeks or months for side effects to stop.
Exercise and eating healthy food can help you feel better.

You might worry about cancer and side effects.
You can talk to:
- a doctor
- your family or friends
- a counsellor.

More Easy Read resources
This Easy Read information was published in July 2025 and funded through the generosity of a Perpetual IMPACT grant.
We thank the health professionals, other experts, and people affected by cancer who reviewed this Easy Read information: Prof Deborah Bateson AM, Professor of Practice, Sydney Medical School, Faculty of Medicine and Health, The University of Sydney; Diane Davey, Operations Manager Cancer Services, Albury Wodonga Regional Cancer Centre; A/Prof Fiona Day, Medical Oncologist, Calvary Mater Newcastle; Dr Annie Ho, Radiation Oncologist, Macquarie University Hospital, Mater Hospital and St Vincent’s Hospital; Maha Kamil, Cancer Council Liaison South Western Sydney; Laila Khan, Lead, Cancer Council Liaisons – Greater Sydney, Cancer Council NSW; Elfa Moraitakis, Chief Executive Officer, SydWest Multicultural Services; Dana Mouwad, Director, Statewide Health Literacy Lab; A/Prof Danielle Muscat, Director of Research, NSW Statewide Health Literacy Hub and Applied and Translational Research Lead, Sydney Health Literacy Lab; Jenny Nguyen, Community Fundraising Coordinator, Cancer Council NSW; Dr Abhijit Pal, Medical Oncologist, Liverpool Hospital and Bankstown Hospital; Kate Pallot, Lead Cancer Council Liaison Regional and Rural, Cancer Council NSW; Dukopi Redamwang, Consumer; Amparo Rojo, Consumer; Rafi Sharif, Consumer; Dr Jess Smith, Medical Oncologist, GenesisCare Campbelltown; Dr Janelle Weise, Senior Research Fellow, National Centre of Excellence in Intellectual Disability Health (now incorporates 3DN), University of NSW; Dr Lauren Winkler, Post-Doctoral Research Fellow and Study Coordinator ScreenEQUAL Cervical Cancer and HPV Stream, Daffodil Centre.
We also gratefully acknowledge the contributions of all focus group participants from Arab Council Australia and SydWest Multicultural Services who generously shared their time, experiences and perspectives.
This content was assessed using the SHeLL Health Literacy Editor, a tool developed by the Sydney Health Literacy Lab to evaluate and improve the clarity of written health information: Ayre J., Bonner C., Muscat D.M., Dunn A.G., Harrison E., Dalmazzo J., Mouwad D., Aslani P., Shepherd H.L., McCaffery K.J., “Automated Health Literacy Assessments of Written Health Information: Development of the SHeLL (Sydney Health Literacy Lab) Health Literacy Editor v1”, JMIR Formative Research, 2023, e40645. DOI: 10.2196/40645.
View the Cancer Council NSW editorial policy.