- Home
- Brain tumours
- Treatment
- Radiation therapy
Radiation therapy for brain cancer
Also known as radiotherapy, radiation therapy uses a controlled dose of radiation to kill or damage tumour cells in the area being treated. The radiation is usually in the form of x-ray beams.
For more on this, see our general section on Radiation therapy.
Learn more about:
- How radiation therapy is given
- How often will you have it?
- Stereotactic radiosurgery (SRS)
- Stereotactic radiation therapy (SRT)
- Proton therapy
- Wearing an immobilisation mask
- Side effects of radiation therapy
- Video: What is radiation therapy?
How radiation therapy is given
For gliomas, radiation therapy is typically given after surgery, possibly along with chemotherapy (chemoradiation). Before you start radiation therapy, a radiation therapist will take measurements of your body and do a CT and/or MRI scan to work out the precise area to be treated.
Treatment is carefully planned to do as little harm as possible to the healthy brain tissue near the tumour. Radiation therapy itself is painless, though you may experience some side effects. Your treatment team will discuss these with you before you begin treatment.
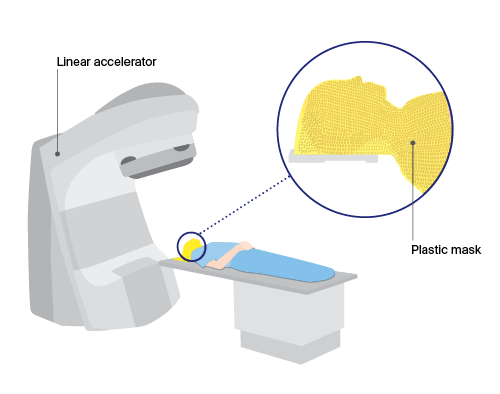
If you are having radiation therapy for a brain tumour, you will probably need to wear a special plastic mask over your face. If you are having radiation therapy for a spinal cord tumour, some small marks may be tattooed on your skin to show the treatment area.
For glioblastomas (grade 4 cancers), radiation therapy is usually combined with chemotherapy. This is called chemoradiation. The chemotherapy drugs make the cancer cells more sensitive to radiation therapy.
How often will you have it?
How often you have radiation therapy (the treatment course) will depend on the size and type of tumour. Usually it is given once a day, from Monday to Friday, for several weeks. During treatment, you will lie on a table under a machine called a linear accelerator (LINAC). Most machines use imaging scans to check you are in the correct position for treatment. Each daily treatment will last for about 10–15 minutes.
Stereotactic radiosurgery (SRS)
Stereotactic radiosurgery (SRS) is a specialised type of radiation therapy, not a type of surgery, and no cuts are made in the skull.
A specialised radiation machine is used to give very precisely targeted radiation to the tumour. Machine types include LINAC, GammaKnife and CyberKnife. They deliver a high dose of radiation to the tumour while the surrounding healthy brain tissue receives very little.
SRS is not suitable for all types of brain tumours. It may be offered when neurosurgery is not possible or as an alternative to neurosurgery. It is most commonly used for cancers that have spread to the brain from another part of the body. It is also used for some meningiomas, pituitary tumours and schwannomas, and is occasionally used for gliomas that have come back after other treatment.
Often, only 1–5 doses of SRS are needed. A treatment session may last between 15 minutes and two hours, depending on the type of radiosurgery given. You will need to wear a special mask or frame during the treatment. You will usually be able to go home afterwards.
Stereotactic radiation therapy (SRT)
A stereotactic radiosurgery machine may also be used to deliver a longer course of radiation, particularly for benign brain tumours. This is called stereotactic radiation therapy. The treatment is given as multiple small daily doses.
If you feel anxious before your radiation therapy sessions, you may find it helpful to listen to the meditation and relaxation exercises in our Finding Calm During Cancer podcast.
Wearing an immobilisation mask
You’ll need to wear a plastic mask during radiation therapy to the brain. This is known as an immobilisation mask. It will help keep your head still and make sure the radiation is targeted at the same area during each session. The mask is made to fit you. It is fixed to the table while the treatment is delivered.
The mask is made of a tight‑fitting mesh, but you will wear it for only about 10 minutes at a time. You can see, speak and breathe through the mask, but it may feel strange and confined at first. Tell the radiation therapists if wearing the mask makes you feel anxious. With the support of the radiation therapy team, many people find that they get used to wearing the mask. The team may suggest you try breathing or relaxation exercises, or you may be offered medicine to help you relax.
Proton therapy
This uses protons rather than x‑ray beams. Protons are tiny parts of atoms with a positive charge. Proton therapy is useful for some types of brain and spinal cord tumours, and tumours near sensitive areas. It is not yet available in Australia (as at mid 2022), but there is funding in special cases to allow Australian to travel overseas for treatment.
Side effects of radiation therapy
Radiation therapy side effects generally occur in the treatment area. They are usually temporary, but some may last for a few months or years, or be permanent. The side effects vary depending on whether the tumour is in the brain or spinal cord. They may include:
- nausea – can occur several hours after treatment
- headaches – can occur during the course of treatment
- tiredness or fatigue – worse at the end of the treatment course; can continue to build after treatment, but usually improves over a month or so
- dry, itchy, red, sore or flaky skin – may occur in the treatment area; usually happens at the end of the treatment course and lasts 1–2 weeks before going away
- hair loss – may occur in a patch in the area of the head receiving treatment; usually temporary but in some cases permanent; if hair grows back, the texture or colour may be different
- dulled hearing – may occur if fluid builds up in the middle ear and may be permanent.
Radiation therapy side effects specific for spinal cord tumours include swallowing problems (dysphagia) if the neck is treated and diarrhoea if the lower spine is treated. Both are temporary.
If any side effects develop, talk to your radiation oncology team. They can suggest ways to manage them.
A small number of adults who have had radiation therapy to the brain have side effects that appear months or years after treatment. These are called late effects and can include symptoms such as poor memory, confusion and headaches. The problems that might develop depend on the part of the brain that was treated.
High-dose radiation to the pituitary gland can cause it to produce too little of some hormones. This can affect body temperature, growth, sleep, weight and appetite. The hormone levels in your pituitary gland will be monitored during and after treatment.
→ READ MORE: Chemotherapy for brain cancer
Video: Radiation therapy for brain cancer
Watch this video to learn more about how radiation therapy is used to treat brain tumours.
Podcast: Making treatment decisions
Listen now
More resources
A/Prof Lindy Jeffree, Neurosurgeon, Royal Brisbane and Women’s Hospital, QLD; Emma Daly, Neuro-oncology Clinical Nurse Consultant, Cabrini Health, VIC; A/Prof Andrew Davidson, Neurosurgeon, Victorian Gamma Knife Service, Peter MacCallum Cancer Centre and Department of Neurosurgery, Royal Melbourne Hospital, VIC; Beth Doggett, Consumer; Kate Fernandez, 13 11 20 Consultant, Cancer Council SA; Melissa Harrison, Allied Health Manager and Senior Neurological Physiotherapist, Advance Rehab Centre, NSW; A/Prof Rosemary Harrup, Director, Cancer and Blood Services, Royal Hobart Hospital, TAS; A/Prof Eng-Siew Koh, Radiation Oncologist, Liverpool Cancer Therapy Centre, Liverpool Hospital and University of New South Wales, NSW; Andy Stokes, Consumer.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.
Need to talk?
Support services
Coping with cancer?
Speak to a health professional or to someone who has been there, or find a support group or forum
Need legal and financial assistance?
Pro bono services, financial and legal assistance, and no interest loans
Cancer information
Making cancer treatment decisions
Decision-making steps, consent and second opinions
What is radiation therapy?
Key questions about radiation therapy as part of cancer treatment