- Home
- Anal cancer
- About anal cancer
About anal cancer
Anal cancer is cancer affecting the tissues of the anus, the opening at the end of the bowel.
Learn more:
Overview
Anal cancer affects the tissues of the anus. It can start in any part of the anus including the anal margin, anal canal and transitional zone. Cancer is a disease of the cells. Cells are the body’s basic building blocks – they make up tissues and organs. The body constantly makes new cells to help us grow, replace worn-out tissue and heal injuries.
Normally, cells multiply and die in an orderly way, with each new cell replacing one lost. Sometimes cells become abnormal and keep growing. These abnormal cells may form a lump or tumour. If the cells in a tumour are cancerous, they can spread through the bloodstream or lymph vessels and form another tumour at a new site. This new tumour is known as secondary cancer or metastasis.
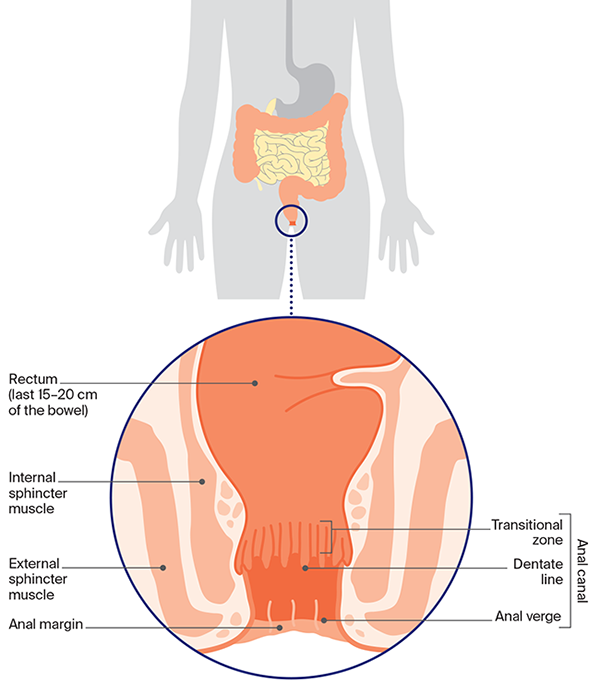
About the anus
The anus is the opening at the end of the large bowel. It is made up of the last few centimetres of the bowel (anal canal) and the skin around the opening (anal margin). During a bowel movement, the anus muscles (sphincters) relax to release the solid waste matter known as faeces, stools or poo.
Structure of the anus
Types of anal cancer
| squamous cell carcinoma (SCC) | Most anal cancers are SCCs. These start in the flat (squamous) cells that line much of the anus. The term “anal cancer” commonly refers to SCCs, and this fact sheet focuses on this type of anal cancer. |
| adenocarcinoma | This is a less common type of anal cancer. Adenocarcinomas can start in cells that line the upper part of the anus near the rectum or in the glands that release secretions into the anal canal. It can be treated in a similar way to bowel cancer. |
| skin cancer | In rare cases, SCCs can affect the skin just outside the anus. These are called anal margin SCCs. If they are not too close to the sphincter muscles, they can be treated in a similar way to SCCs on other areas of the skin. For more on this, see Skin cancer. |
Who gets anal cancer?
Every year, about 615 people are diagnosed with anal cancer in Australia. It is more common over the age of 50 and more women than men are diagnosed with it. The number of people diagnosed with anal cancer has increased over recent decades.
While anal cancer is rare (fewer than 2 cases in 100,000 people), rates are more than 40 times higher in gay and bisexual men and other men who have sex with men.
See LGBTQI+ people and cancer or visit The Bottom Line for specific information.
What causes anal cancer?
About 90% of anal cancers are caused by infection with specific strains of a very common virus called human papillomavirus (HPV). HPV can infect the surface of different areas, including the anus, cervix, vulva, vagina, penis, mouth and throat. Some HPV strains cause anal and genital warts.
About 4 out of 5 people will become infected with one type of genital HPV at some time in their lives. Unless they are tested, most people won’t know they have an HPV infection as it usually doesn’t cause symptoms. If cancer develops, it usually appears many years after the first infection.
Other risk factors for anal cancer include:
- having a weakened immune system, e.g. because of human immunodeficiency virus (HIV) infection, an organ transplant or an autoimmune disease such as coeliac disease, lupus or Graves disease
- being a receptive partner (“bottom”) in anal sex
- having anal or genital warts
- having had an abnormal cervical screening test
- having had cancer of the cervix, vulva or vagina
- smoking tobacco
- having unprotected sex
- having many sex partners
- being aged over 45.
People diagnosed with anal cancer may not have any of these risk factors.
Vaccination can prevent infection with HPV. The most common HPV vaccine used in Australia protects against cancers linked with HPV including anal, cervical, vaginal and vulvar cancers. Under the national HPV vaccination program, free vaccines are provided at school for all children aged 12–13. Visit hpvvaccine.org.au to see who else is eligible for free vaccination.
→ READ MORE: Anal cancer symptoms
More resources
Glen Guerra, Colorectal Surgeon, Peter MacCallum Cancer Centre and St Vincents Hospital Melbourne, VIC; Holly Davey, 13 11 20 Consultant, Cancer Council Queensland; Prof Peter Gibbs, Laboratory Head, Walter and Eliza Hall Institute, The University of Melbourne, Medical Oncologist, Western Hospital, VIC; A/Prof Ian Faragher, The University of Melbourne, Head of Colorectal and General Surgery Unit, Western Health, VIC; Justin Hargreaves, Medical Oncology Nurse Practitioner, Bendigo Health Cancer Centre, VIC; Prof Richard Hillman, Senior Staff Specialist, HIV and Immunology, St Vincent’s Health Network, Sydney, Conjoint Professor, St Vincent’s Clinical Campus and The Kirby Institute, NSW; A/Prof George Hruby, Radiation Oncologist, Royal North Shore Hospital, Visiting Radiation Oncologist, Genesiscare and Dubbo Base Hospital, NSW; Annie Jacobs, Consumer; Mariad O’Gorman, Clinical Psychologist, Bankstown Cancer Therapy Centre, NSW; Terry Scully, Consumer.
View the Cancer Council NSW editorial policy.
View all publications or call 13 11 20 for free printed copies.